Abstract
Introduction Asymptomatic neutropenia is a common referral to Hematology. Differentiating between a normal variant and an underlying hematologic disorder is further complicated by discrepancies in blood cell count reference ranges that differ among institutions. In the following study, we aim to describe the demographic characteristics and laboratory and clinical outcomes of patients referred for asymptomatic neutropenia to an academic classical hematology practice.
Methods In this retrospective cohort study, we included all adult patients referred for evaluation of asymptomatic neutropenia to the Classical Hematology Clinic at Oregon Health & Science University from 2018 through 2021. Asymptomatic neutropenia was defined as an absolute neutrophil count (ANC) below the internal reference range of 1.8 x 109/L, without a history of abnormal infection. Patients who had other cytopenias were included in the study as long as the primary referral reason was asymptomatic neutropenia. Patient demographics, pertinent medical history, baseline laboratory values, diagnostic testing and results, and subsequent clinical diagnoses were obtained through individual chart review. A clinically significant outcome was defined as a newly diagnosed hematologic disorder, including both pre-malignant and malignant conditions. Standard descriptive statistics were used to summarize baseline and outcome characteristics.
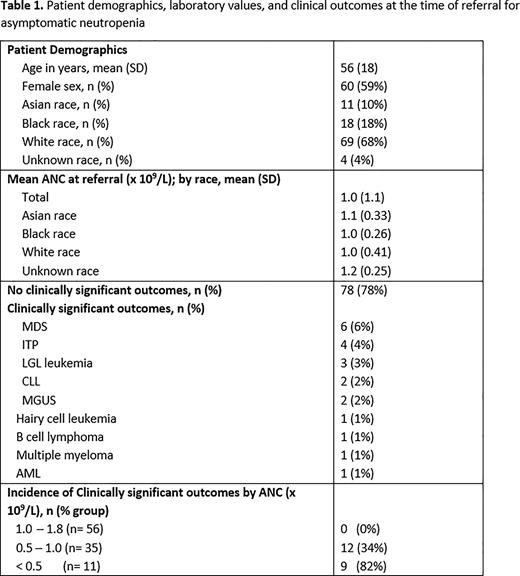
Results We identified 102 patients who were referred over the 3-year period and who met the study inclusion criteria. The median age was 56 years (range: 19 - 96), 10% of patients identified as Asian, 18% as Black, and 68% as White (Table 1), which was disproportionate to local population demographics in Portland Oregon (9% Asian, 6% Black, and 75% White). The average ANC at referral was 1.0 x 109/L. 55% of patients had an ANC between 1.8 x 109/L - 1.0 x 109/L, 34% had an ANC between 1.0 x 109/L - 0.5 x 109/L and 11% had an ANC less than 0.5 x 109/L. The average number of tests performed at referral, including repeat complete blood cell count with differential, was 6. Bone marrow biopsies were obtained in 15 patients who had an average ANC 0.6 x 109/L (standard deviation 0.46). The most common clinical outcome was idiopathic persistent neutropenia in 50% of patients, with resolution of neutropenia in occurring in 28% of patients. Among patients with an ANC > 1.0 x 109/L, only 1 patient was found to have a clinically relevant underlying disorder (HIV infection). In total, twenty-three percent of patients were found to have a clinically significant outcome with mean ANC of 0.65 x 109/L: Myelodysplastic syndrome (n=6), Immune thrombocytopenic purpura (n=4), Large granular lymphocytic leukemia (LGL) (n=3), Chronic lymphocytic leukemia (n=2), monoclonal gammopathy of undetermined significance (MGUS) (n=2), Hairy cell leukemia (n=1), B cell lymphoma (n=1), Multiple myeloma (n=1), and Acute Myeloid Leukemia (n=1). Only two of these patients with clinically significant findings (MGUS and LGL leukemia) were Black. Among Black patients who underwent testing for Duffy antigens, nearly 100% of patients were positive for the Duffy null phenotype [Fy(a-b-)], though one patient was [Fy(a-b+)]. In Non-Black patients tested, only 25% were positive for this phenotype.
Conclusion Among patients referred to our institution for asymptomatic neutropenia, none of the patients with ANC > 1.0 x 109/L had an underlying hematologic disorder detectable by standard peripheral blood neutropenia workup. Black individuals were disproportionately represented, more likely to harbor the Duffy null phenotype, and less likely to have a clinically significant outcome. Our findings elucidate the need for standardized reference ranges that include demographic variants and are more representative of the community they serve, as current thresholds may inadvertently flag benign as abnormal, leading to significant emotional and financial implications, as well as inequitable treatment decision-making.
Abbreviations: ANC, absolute neutrophil count; CBC, complete blood cell count; MDS, Myelodysplastic syndrome; ITP, Immune thrombocytopenic purpura; LGL, Large granular lymphocytic leukemia; CLL, Chronic lymphocytic leukemia; MGUS, monoclonal gammopathy of undetermined significance; AML, Acute myeloid leukemia
Disclosures
Shatzel:Aronora, Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal